Table of Contents
Brief Explanation of Autoimmune Diseases
Autoimmune diseases occur when the body’s immune system mistakenly attacks its own tissues. Normally, the immune system defends against harmful invaders like bacteria and viruses. However, in autoimmune conditions, this defense mechanism becomes misdirected, leading to inflammation and damage in various organs and tissues. There are over 80 known autoimmune diseases, each affecting different parts of the body and presenting a unique set of challenges.
Importance of Understanding These Conditions
Understanding autoimmune diseases is crucial for several reasons. First, they often present with a wide range of symptoms that can be difficult to diagnose. Early and accurate diagnosis is essential for effective management and treatment. Second, autoimmune diseases can significantly impact a person’s quality of life, making it vital for patients, caregivers, and the general public to be aware of the symptoms, causes, and available treatments. Awareness can also lead to better support, improved research funding, and more comprehensive care strategies.
Overview of What the Blog Will Cover
This blog aims to provide a comprehensive overview of autoimmune diseases, starting with a detailed explanation of what they are and how they disrupt the immune system. We will explore several common autoimmune diseases, highlighting their symptoms, causes, and risk factors. The blog will also cover diagnostic methods, treatment options, and strategies for managing life with an autoimmune condition. By the end, readers will have a clearer understanding of these complex diseases and how to navigate their challenges.
What Are Autoimmune Diseases?
Definition of Autoimmune Diseases
Autoimmune diseases are a group of disorders where the immune system mistakenly targets and attacks the body’s own cells and tissues. In a healthy immune system, the body is able to distinguish between foreign invaders, such as bacteria and viruses, and its own cells. In autoimmune diseases, this distinction fails, leading the immune system to mount an inappropriate response against the body’s own tissues, resulting in inflammation and damage.
How the Immune System Typically Works
The immune system is a complex network of cells, tissues, and organs that work together to protect the body from harmful pathogens. It identifies and eliminates threats through a highly organized process:
- Recognition: Immune cells recognize pathogens based on specific markers called antigens.
- Response: When a pathogen is detected, the immune system deploys various cells and molecules to neutralize and remove it.
- Regulation: After the threat is eliminated, the immune system scales back the response to prevent damage to healthy tissues.
This system is normally highly regulated, with checks and balances to prevent it from attacking the body’s own cells.
How Autoimmune Diseases Alter Immune Response
In autoimmune diseases, the immune system’s regulatory mechanisms fail, leading to the following issues:
- Loss of Self-Tolerance: The immune system loses its ability to recognize the body’s own cells as “self,” leading to an attack on these cells. This loss of self-tolerance can be due to genetic factors, environmental triggers, or a combination of both.
- Inappropriate Immune Response: The immune system generates antibodies or immune cells that target the body’s own tissues, leading to chronic inflammation and tissue damage. This response is often misguided and persistent, causing ongoing harm to the affected organs or systems.
- Autoantibody Production: Many autoimmune diseases involve the production of autoantibodies—antibodies that mistakenly target and react with a person’s own tissues. These autoantibodies can contribute to tissue destruction and disease progression.
Overall, autoimmune diseases represent a significant deviation from normal immune function, leading to a range of symptoms and potential damage to various body parts.
Common Autoimmune Diseases
Overview of Several Common Autoimmune Diseases
Autoimmune diseases can affect different parts of the body, and each condition has its own unique characteristics. Here’s a brief overview of some of the most common autoimmune diseases:
1. Rheumatoid Arthritis (RA)
- Description: Rheumatoid arthritis is a chronic inflammatory disorder that primarily affects the joints. It leads to pain, swelling, and eventually joint damage. RA can also impact other organs, such as the skin, eyes, and lungs.
- Key Statistics: RA affects approximately 1% of the global population. It is more common in women, with about two to three times as many women affected compared to men. Onset typically occurs between the ages of 30 and 60.
2. Lupus (Systemic Lupus Erythematosus – SLE)
- Description: Lupus is a systemic autoimmune disease where the immune system attacks multiple organs and systems, including the skin, joints, kidneys, and heart. Symptoms can be diverse and may include a butterfly-shaped facial rash, joint pain, and extreme fatigue.
- Key Statistics: Lupus affects around 5 million people worldwide, with the majority being women, particularly those of African, Hispanic, and Asian descent. It often develops between the ages of 15 and 44.
3. Multiple Sclerosis (MS)
- Description: Multiple sclerosis is a disease where the immune system attacks the protective sheath (myelin) covering nerve fibers in the central nervous system. This leads to communication problems between the brain and the rest of the body. Symptoms vary widely and can include vision problems, muscle weakness, and difficulties with coordination and balance.
- Key Statistics: MS affects about 2.8 million people globally. It is more prevalent in women than men and commonly begins between the ages of 20 and 40. MS is more common in people living in temperate climates, such as those in Europe and North America.
4. Type 1 Diabetes (T1D)
- Description: Type 1 diabetes is an autoimmune disease in which the immune system attacks insulin-producing cells in the pancreas, leading to high blood sugar levels. People with T1D require lifelong insulin therapy to manage their blood sugar.
- Key Statistics: Type 1 diabetes affects approximately 1 in 300 people in the United States and 1 in 1,000 people in Europe. It often begins in childhood or adolescence but can occur at any age.
5. Hashimoto’s Thyroiditis
- Description: Hashimoto’s thyroiditis is an autoimmune disorder where the immune system attacks the thyroid gland, leading to hypothyroidism (underactive thyroid). Symptoms can include fatigue, weight gain, and sensitivity to cold.
- Key Statistics: Hashimoto’s thyroiditis is the most common cause of hypothyroidism and affects about 5% of the population in the United States, with a higher prevalence in women.
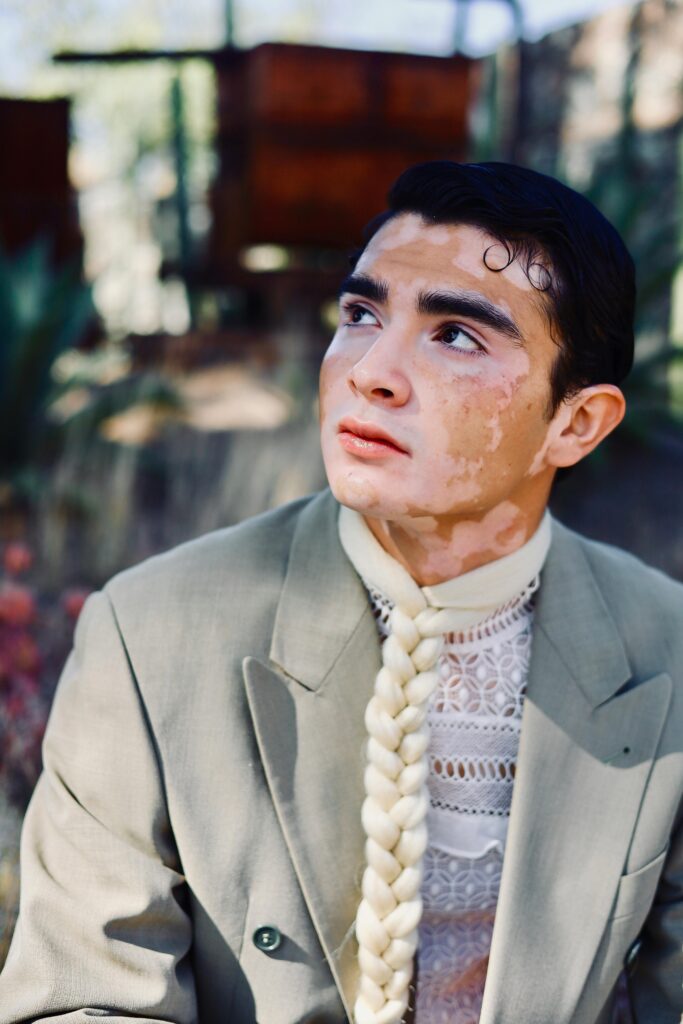
6. Psoriasis
- Description: Psoriasis is a chronic skin condition characterized by red, scaly patches on the skin. It results from the rapid growth of skin cells and is often accompanied by joint pain (psoriatic arthritis).
- Key Statistics: Psoriasis affects approximately 2% of the global population. It is equally common in men and women and often begins in early adulthood.
Prevalence and Impact
Autoimmune diseases collectively affect millions of people worldwide, with a significant impact on quality of life and healthcare systems. The prevalence of these conditions varies by region, age, and gender, with many autoimmune diseases more common in women than men. Early diagnosis and appropriate management are crucial for improving outcomes and quality of life for those affected.
Symptoms of Autoimmune Diseases
General Symptoms Common Across Autoimmune Diseases
Many autoimmune diseases share overlapping symptoms due to the nature of immune system dysfunction and inflammation. Common general symptoms include:
- Fatigue: Persistent and often debilitating tiredness that doesn’t improve with rest. It’s one of the most common symptoms and can affect daily functioning.
- Joint Pain and Swelling: Many autoimmune diseases involve inflammation of the joints, leading to pain, stiffness, and swelling.
- Skin Issues: Rashes, itching, and lesions can occur, as seen in conditions like psoriasis and lupus. These skin manifestations are often a direct result of immune system activity.
- Fever: Low-grade fever is common in many autoimmune diseases and is often a sign of inflammation or infection.
- Muscle Weakness: Muscle pain or weakness can occur, particularly in diseases that affect the muscles or nerves.
Disease-Specific Symptoms
- Rheumatoid Arthritis (RA):
- Joint Swelling: RA typically causes swelling in the joints, which can lead to visible puffiness and discomfort. The swelling often affects multiple joints simultaneously.
- Morning Stiffness: People with RA often experience stiffness in their joints upon waking, which can last for an extended period and improve as the day progresses.
- Lupus (Systemic Lupus Erythematosus – SLE):
- Butterfly-Shaped Rash: A distinctive facial rash that spreads across the cheeks and nose, resembling a butterfly. This rash is characteristic but not present in all cases.
- Fever: Unexplained fevers can occur and are often a sign of active disease. They can fluctuate and may be associated with flare-ups.
- Multiple Sclerosis (MS):
- Muscle Weakness: Individuals with MS may experience varying degrees of muscle weakness, which can affect mobility and daily activities.
- Vision Problems: Common issues include blurred vision, double vision, or loss of vision in one eye. These symptoms are due to damage to the optic nerves.
How Symptoms May Vary by Individual and Disease Stage
- Individual Variation: The presentation of autoimmune diseases can vary widely between individuals. Some may experience mild symptoms that are manageable, while others may have severe manifestations. The severity and type of symptoms can be influenced by factors such as genetics, overall health, and the presence of other conditions.
- Disease Stage: Symptoms can also change depending on the stage of the disease. For instance:
- Early Stage: Symptoms may be less severe and more generalized, making diagnosis challenging. Early symptoms might include vague discomfort or fatigue.
- Active Stage: During flare-ups, symptoms can become more intense and noticeable. Inflammatory responses are heightened, leading to more pronounced pain, swelling, or other issues.
- Remission Stage: Some autoimmune diseases have periods of remission where symptoms are lessened or disappear entirely. However, symptoms may recur later, and the disease can fluctuate in severity.
Overall, the symptom profile of autoimmune diseases is diverse and can evolve over time. Recognizing these symptoms and understanding their variability is crucial for effective management and treatment.
Causes and Risk Factors
Genetic Predisposition and Family History
Genetics play a significant role in the development of autoimmune diseases. Many autoimmune conditions show a familial pattern, suggesting a hereditary component:
- Genetic Susceptibility: Certain genes are associated with a higher risk of developing autoimmune diseases. For example, specific variations in genes related to immune system regulation and response may predispose individuals to these conditions.
- Family History: Individuals with a family history of autoimmune diseases are at a higher risk of developing similar conditions. This familial tendency highlights the importance of genetic factors in autoimmune disease development.
Environmental Triggers
Environmental factors can trigger or exacerbate autoimmune diseases in individuals who are genetically predisposed:
- Infections: Certain infections can prompt an autoimmune response by causing the immune system to attack not only the pathogen but also the body’s own tissues. Examples include viral infections like Epstein-Barr virus and bacteria like Mycobacterium tuberculosis.
- Toxins: Exposure to environmental toxins, such as heavy metals or certain chemicals, can also trigger autoimmune responses. Long-term exposure to pollutants or industrial chemicals may increase the risk of developing autoimmune diseases.
- Diet and Gut Microbiota: Emerging research suggests that dietary factors and imbalances in gut microbiota may influence the onset and progression of autoimmune diseases.
Hormonal Factors and Gender Differences
Hormones, particularly sex hormones, play a role in the development and progression of autoimmune diseases:
- Hormonal Influence: Autoimmune diseases are often more common in women, which suggests that hormones such as estrogen may influence immune system function and autoimmune disease risk. For instance, autoimmune diseases like lupus and rheumatoid arthritis are more prevalent in women, especially during their reproductive years.
- Hormonal Fluctuations: Hormonal changes during pregnancy, menstruation, and menopause may affect disease activity and progression. Some autoimmune diseases may flare up or improve in response to these hormonal fluctuations.
Lifestyle Factors and Their Impact
Certain lifestyle factors can influence the risk and severity of autoimmune diseases:
- Stress: Chronic stress is known to impact immune function and may contribute to the development or exacerbation of autoimmune conditions. Stress management techniques can be beneficial in managing autoimmune diseases.
- Diet and Nutrition: A balanced diet with adequate nutrients supports overall health and may help manage autoimmune symptoms. Certain diets, such as those rich in anti-inflammatory foods, might have a positive impact on autoimmune disease management.
- Physical Activity: Regular physical activity can help maintain overall health, reduce inflammation, and improve quality of life for individuals with autoimmune diseases. However, excessive or inappropriate exercise may worsen symptoms for some individuals.
Overall, autoimmune diseases result from a complex interplay of genetic, environmental, hormonal, and lifestyle factors. Understanding these causes and risk factors can help in managing and potentially mitigating the impact of autoimmune diseases.
Diagnosis of Autoimmune Diseases
Overview of Diagnostic Methods
Diagnosing autoimmune diseases involves a combination of methods to accurately identify the condition and differentiate it from other illnesses. Common diagnostic approaches include:
- Blood Tests: Blood tests are crucial for diagnosing autoimmune diseases. They often include:
- Autoantibody Tests: These detect specific antibodies produced by the immune system that target the body’s own tissues. Examples include antinuclear antibodies (ANA) for lupus and rheumatoid factor (RF) for rheumatoid arthritis.
- Inflammatory Markers: Tests like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) measure levels of inflammation in the body.
- Complete Blood Count (CBC): This test assesses overall health and detects conditions such as anemia or signs of infection.
- Imaging: Imaging techniques help visualize internal structures and detect damage or inflammation:
- X-rays: Useful for assessing joint damage in conditions like rheumatoid arthritis.
- Ultrasound: Can be used to examine soft tissues and joints for inflammation or damage.
- Magnetic Resonance Imaging (MRI): Provides detailed images of soft tissues and is helpful in diagnosing conditions like multiple sclerosis by revealing lesions in the brain and spinal cord.
- Biopsies: In some cases, a tissue biopsy may be necessary to confirm a diagnosis. A small sample of tissue is removed and examined under a microscope:
- Skin Biopsy: Often used to diagnose skin conditions like psoriasis or lupus.
- Organ Biopsies: May be performed if the disease affects organs such as the kidneys or liver.
Challenges in Diagnosis
Diagnosing autoimmune diseases can be challenging due to several factors:
- Symptom Overlap: Many autoimmune diseases have symptoms that overlap with other conditions, making it difficult to pinpoint the exact diagnosis. For instance, fatigue and joint pain can be seen in multiple autoimmune disorders as well as other illnesses.
- Variable Presentation: Symptoms can vary widely among individuals with the same autoimmune disease, and disease progression can also differ. This variability can complicate the diagnostic process.
- Lack of Specific Tests: Some autoimmune diseases lack specific diagnostic tests, relying instead on a combination of clinical symptoms and laboratory findings. This can lead to delays in diagnosis or misdiagnosis.
Importance of Early Diagnosis and Ongoing Monitoring
- Early Diagnosis: Early identification of autoimmune diseases is critical for effective treatment and management. Early intervention can help prevent or minimize damage to affected tissues and improve long-term outcomes. It also allows for better management of symptoms and potential disease complications.
- Ongoing Monitoring: Autoimmune diseases often require continuous monitoring to assess disease progression and response to treatment. Regular follow-up visits, blood tests, and imaging may be necessary to adjust treatment plans and manage flare-ups or complications.
- Preventive Measures: Regular monitoring can also help in identifying and addressing potential side effects of treatments, as well as implementing preventive measures to maintain overall health and well-being.
Overall, a comprehensive diagnostic approach and ongoing management are essential in effectively addressing autoimmune diseases and improving the quality of life for those affected.
Treatments and Management
General Treatment Approaches
- Medications: Medications are commonly used to manage autoimmune diseases, reduce inflammation, and suppress the overactive immune response. They may include:
- Anti-inflammatory Drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs) help reduce pain and inflammation.
- Immunosuppressants: These drugs suppress the immune system’s activity to prevent it from attacking the body’s tissues. Examples include methotrexate and azathioprine.
- Lifestyle Changes: Adapting lifestyle habits can significantly impact disease management:
- Diet: A balanced diet rich in anti-inflammatory foods (such as fruits, vegetables, and omega-3 fatty acids) can help manage symptoms. Avoiding foods that trigger inflammation may also be beneficial.
- Exercise: Regular physical activity helps maintain overall health, manage symptoms, and improve mobility and flexibility.
- Stress Management: Techniques such as mindfulness, meditation, and relaxation exercises can help manage stress, which may exacerbate autoimmune symptoms.
Disease-Specific Treatments
- Rheumatoid Arthritis (RA):
- Disease-Modifying Antirheumatic Drugs (DMARDs): Medications like methotrexate and sulfasalazine slow disease progression and prevent joint damage.
- Biologics: These are advanced drugs that target specific parts of the immune system. Examples include tumor necrosis factor (TNF) inhibitors like etanercept and adalimumab.
- Lupus:
- Corticosteroids: These drugs reduce inflammation and control symptoms. Commonly used corticosteroids include prednisone.
- Antimalarial Drugs: Medications such as hydroxychloroquine help manage symptoms and prevent flares by modulating the immune response.
- Multiple Sclerosis (MS):
- Disease-Modifying Therapies (DMTs): These drugs, such as interferon beta and glatiramer acetate, help reduce the frequency and severity of MS relapses and slow disease progression.
- Physical Therapy: Rehabilitation and physical therapy help improve mobility, strength, and balance, addressing the physical impairments associated with MS.
Role of Diet, Exercise, and Mental Health in Managing Symptoms
- Diet: Adopting an anti-inflammatory diet can help manage symptoms and reduce flare-ups. Nutrient-rich foods and proper hydration support overall health and can alleviate some autoimmune symptoms.
- Exercise: Regular exercise improves overall health, helps maintain a healthy weight, reduces stress, and can ease symptoms like joint pain and fatigue. It is important to tailor exercise routines to individual abilities and limitations.
- Mental Health: Addressing mental health through therapy, counseling, or support groups is crucial. Coping with a chronic illness can be emotionally challenging, and mental health support can improve overall well-being and resilience.
Emerging Treatments and Research Developments
- Biological Therapies: New biologic drugs are continually being developed to target specific immune system components with greater precision, aiming to reduce side effects and improve efficacy.
- Personalized Medicine: Advances in genomics and personalized medicine are leading to more tailored treatments based on an individual’s genetic profile and specific disease characteristics.
- Novel Therapies: Research into new treatment modalities, such as stem cell therapy and gene editing, holds promise for more effective management and potential cures for some autoimmune diseases.
Living with Autoimmune Diseases
Strategies for Managing Chronic Symptoms
- Routine Monitoring: Regular check-ups and ongoing assessment of symptoms help manage chronic conditions effectively and adjust treatments as needed.
- Self-Care: Implementing daily routines that accommodate symptoms, such as pacing activities and managing fatigue, can help maintain quality of life.
- Adaptive Techniques: Using assistive devices or modifying the home environment can improve functionality and independence.
Importance of Support Networks
- Support Groups: Joining support groups provides emotional support, practical advice, and a sense of community. Connecting with others who have similar experiences can be reassuring and informative.
- Counseling: Professional counseling or therapy can help individuals cope with the emotional and psychological challenges of living with a chronic illness.
Coping Mechanisms and Quality of Life Considerations
- Coping Mechanisms: Developing healthy coping strategies, such as mindfulness, relaxation techniques, and hobbies, can enhance emotional resilience and manage stress.
- Quality of Life: Focusing on activities that bring joy and fulfillment, maintaining social connections, and pursuing personal goals can improve overall quality of life despite the challenges of autoimmune diseases.
Overall, managing autoimmune diseases involves a multifaceted approach that includes medical treatment, lifestyle adjustments, and emotional support. Staying informed about new treatments and maintaining a strong support network are essential for navigating the complexities of living with an autoimmune condition.
Living with Autoimmune Diseases
Strategies for Managing Chronic Symptoms
- Routine Monitoring: Regular medical check-ups and monitoring are essential to track disease progression, manage symptoms, and adjust treatments as necessary. This includes routine blood tests, imaging, and clinical evaluations to keep the condition under control and identify any new or worsening symptoms.
- Medication Adherence: Consistently taking prescribed medications and following treatment plans is crucial for managing autoimmune diseases. It helps control symptoms, reduce flare-ups, and prevent long-term damage.
- Daily Adjustments: Adapting daily routines to accommodate symptoms can make a significant difference. This might include pacing activities to avoid overexertion, using assistive devices for mobility, and modifying home environments to enhance accessibility and comfort.
- Healthy Lifestyle Choices: Incorporating a balanced diet, regular exercise, and adequate sleep into daily life can help manage symptoms and improve overall health. Diet adjustments, such as avoiding foods that trigger inflammation, and engaging in low-impact exercises like swimming or walking, can be beneficial.
- Stress Management: Managing stress through techniques like mindfulness, meditation, and relaxation exercises is important, as stress can exacerbate autoimmune symptoms. Identifying stressors and implementing coping strategies can help reduce their impact.
Importance of Support Networks
- Support Groups: Participating in support groups provides emotional support and practical advice from others with similar experiences. These groups can offer a sense of community, understanding, and shared knowledge about managing the condition.
- Counseling: Professional counseling or therapy can help individuals cope with the emotional and psychological aspects of living with a chronic illness. A counselor can provide strategies for dealing with anxiety, depression, and the stress of managing a long-term condition.
- Family and Friends: Engaging with family and friends for emotional support and practical assistance can be invaluable. Having a strong support system helps with day-to-day challenges and provides encouragement and companionship.
Coping Mechanisms and Quality of Life Considerations
- Coping Mechanisms: Developing effective coping strategies is crucial for managing the emotional and physical challenges of autoimmune diseases. This might include:
- Mindfulness and Relaxation Techniques: Practices such as deep breathing, progressive muscle relaxation, and mindfulness can help manage pain and stress.
- Hobbies and Interests: Engaging in activities and hobbies that bring joy and fulfillment can provide a positive focus and improve overall well-being.
- Quality of Life Considerations: Maintaining a high quality of life despite chronic illness involves:
- Setting Realistic Goals: Setting achievable goals and focusing on what can be controlled helps maintain motivation and a sense of purpose.
- Maintaining Social Connections: Staying connected with friends and family helps prevent isolation and provides emotional support.
- Seeking Joy and Fulfillment: Finding joy in everyday activities and pursuing personal interests and passions can enhance life satisfaction and overall happiness.
Living with autoimmune diseases requires a holistic approach that combines medical management with lifestyle adjustments and emotional support. By adopting effective strategies for symptom management, leveraging support networks, and focusing on quality of life, individuals can navigate the challenges of autoimmune diseases more effectively and lead fulfilling lives.
Conclusion
Recap of Key Points
Autoimmune diseases represent a complex group of disorders where the immune system mistakenly attacks the body’s own tissues. Understanding these conditions involves recognizing their symptoms, such as fatigue, joint pain, and skin issues, and acknowledging the specific manifestations of diseases like rheumatoid arthritis, lupus, and multiple sclerosis. The causes of autoimmune diseases are multifaceted, involving genetic predisposition, environmental triggers, hormonal factors, and lifestyle influences. Diagnosis can be challenging due to symptom overlap and variability, but early diagnosis and ongoing monitoring are critical for effective management. Treatments range from general approaches like medications and lifestyle changes to disease-specific therapies tailored to individual conditions. Managing autoimmune diseases also involves practical strategies for coping with chronic symptoms, utilizing support networks, and maintaining quality of life.
Encouragement for Those Affected to Seek Medical Advice and Support
For individuals affected by autoimmune diseases, seeking timely and accurate medical advice is essential. Consulting with healthcare professionals, including specialists, can provide a clearer diagnosis, effective treatment options, and personalized care plans. Additionally, leveraging support networks such as support groups, counseling, and family and friends can provide invaluable emotional support and practical assistance. Engaging with healthcare providers and support systems can significantly improve disease management and overall well-being.
Call to Action: Staying Informed and Engaged with Ongoing Research
Staying informed about autoimmune diseases and ongoing research is crucial for better management and potential advancements in treatment. Individuals should:
- Stay Updated: Keep up with the latest research, treatment options, and clinical trials related to autoimmune diseases. Reliable sources include medical journals, reputable health organizations, and professional healthcare advice.
- Participate in Research: Consider participating in clinical trials or research studies, if possible. These contributions can help advance understanding and lead to new therapies that may benefit the broader community.
- Advocate for Awareness: Raise awareness about autoimmune diseases within communities and through social platforms. Advocacy can drive better support, funding, and research initiatives.
By remaining engaged and proactive, individuals can play a role in advancing the field of autoimmune disease research and contribute to improved outcomes and quality of life for themselves and others affected by these conditions.
Additional Resources
Links to Relevant Organizations and Support Groups
- American Autoimmune Related Diseases Association (AARDA)
- Website: aarda.org
- Description: AARDA provides information on autoimmune diseases, support resources, and advocacy efforts. It also connects individuals with autoimmune conditions to various support groups and educational materials.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
- Website: niams.nih.gov
- Description: NIAMS, part of the National Institutes of Health (NIH), offers comprehensive information on autoimmune diseases, including research updates, treatment options, and educational resources.
- Lupus Foundation of America
- Website: lupus.org
- Description: This foundation provides support for individuals with lupus, including resources for diagnosis, treatment, and managing daily life with lupus. It also offers information on research and advocacy.
- Multiple Sclerosis Society (NMSS)
- Website: nationalmssociety.org
- Description: The NMSS offers resources for individuals with multiple sclerosis, including information on treatment options, research advancements, and local support groups.
- Rheumatoid Arthritis Support Network (RAS)
- Website: rheumatoidarthritis.net
- Description: RAS provides educational resources, support forums, and tools for managing rheumatoid arthritis. It includes patient stories, treatment options, and expert insights.
Recommended Reading and Websites for Further Information
- “The Autoimmune Solution: Prevent and Reverse the Full Spectrum of Inflammatory Symptoms and Diseases” by Dr. Amy Myers
- Description: This book provides a comprehensive guide to understanding autoimmune diseases, including practical advice on diet, lifestyle changes, and managing symptoms.
- “Lupus: The Essential Guide” by Dr. Robert G. Lahita
- Description: An informative resource on lupus, offering insights into its causes, symptoms, and treatments. It includes advice on managing the disease and living well.
- “Multiple Sclerosis: A Guide for the Newly Diagnosed” by Nancy J. Holland and Nancy L. Sicotte
- Description: This book offers guidance for individuals newly diagnosed with multiple sclerosis, covering treatment options, coping strategies, and daily life adjustments.
- Mayo Clinic’s Autoimmune Diseases Resource
- Website: mayoclinic.org
- Description: The Mayo Clinic provides a broad overview of autoimmune diseases, including symptoms, causes, and treatment options. It also includes tips for managing these conditions.
- WebMD’s Autoimmune Diseases Center
- Website: webmd.com/autoimmune
- Description: WebMD offers detailed information on various autoimmune diseases, including symptoms, diagnosis, and treatment options. It also provides articles and videos on managing autoimmune conditions.
These resources offer valuable information and support for individuals affected by autoimmune diseases, helping them stay informed, connected, and empowered in managing their health.

