Table of Contents
Brief Explanation of COPD
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition characterized by long-term breathing problems and poor airflow. It encompasses two main conditions: chronic bronchitis, which involves a persistent cough and mucus production, and emphysema, which causes damage to the air sacs in the lungs. COPD typically develops over many years and is primarily caused by smoking, though long-term exposure to other irritants can also be a factor. It is a major health concern worldwide, leading to significant morbidity and mortality.
Importance of Understanding COPD
Understanding COPD is crucial for several reasons. First, it is one of the leading causes of death globally, yet it is often underdiagnosed and poorly managed. Recognizing the symptoms and risk factors early can lead to earlier diagnosis and more effective treatment, potentially improving quality of life and slowing disease progression. Furthermore, increasing awareness about COPD can help reduce the stigma associated with the disease and encourage individuals to seek help and make lifestyle changes that can significantly impact their health.
Overview of What the Blog Will Cover
In this blog, we will provide a comprehensive overview of COPD. We will start by defining what COPD is and how it affects the lungs. Next, we’ll explore the causes and risk factors associated with the disease. Understanding the symptoms and how they can vary is crucial for recognizing COPD early. We’ll also discuss the diagnostic process, including the tests used to identify the condition and determine its stage. The blog will cover various treatment and management strategies, from medications to lifestyle changes. Finally, we’ll offer practical advice for living with COPD and discuss prevention strategies to reduce the risk of developing the disease. Our goal is to equip readers with essential knowledge about COPD and empower them to take proactive steps in managing their health.
What is COPD?
Definition of COPD
Chronic Obstructive Pulmonary Disease (COPD) is a term used to describe a group of progressive lung diseases that cause obstructed airflow from the lungs. The primary conditions included under COPD are chronic bronchitis and emphysema. COPD is characterized by long-term breathing difficulties, a persistent cough, and a general decline in lung function. The disease is often progressive, meaning it worsens over time, and is primarily caused by exposure to harmful particles or gases, most commonly from smoking.
Overview of How COPD Affects the Lungs
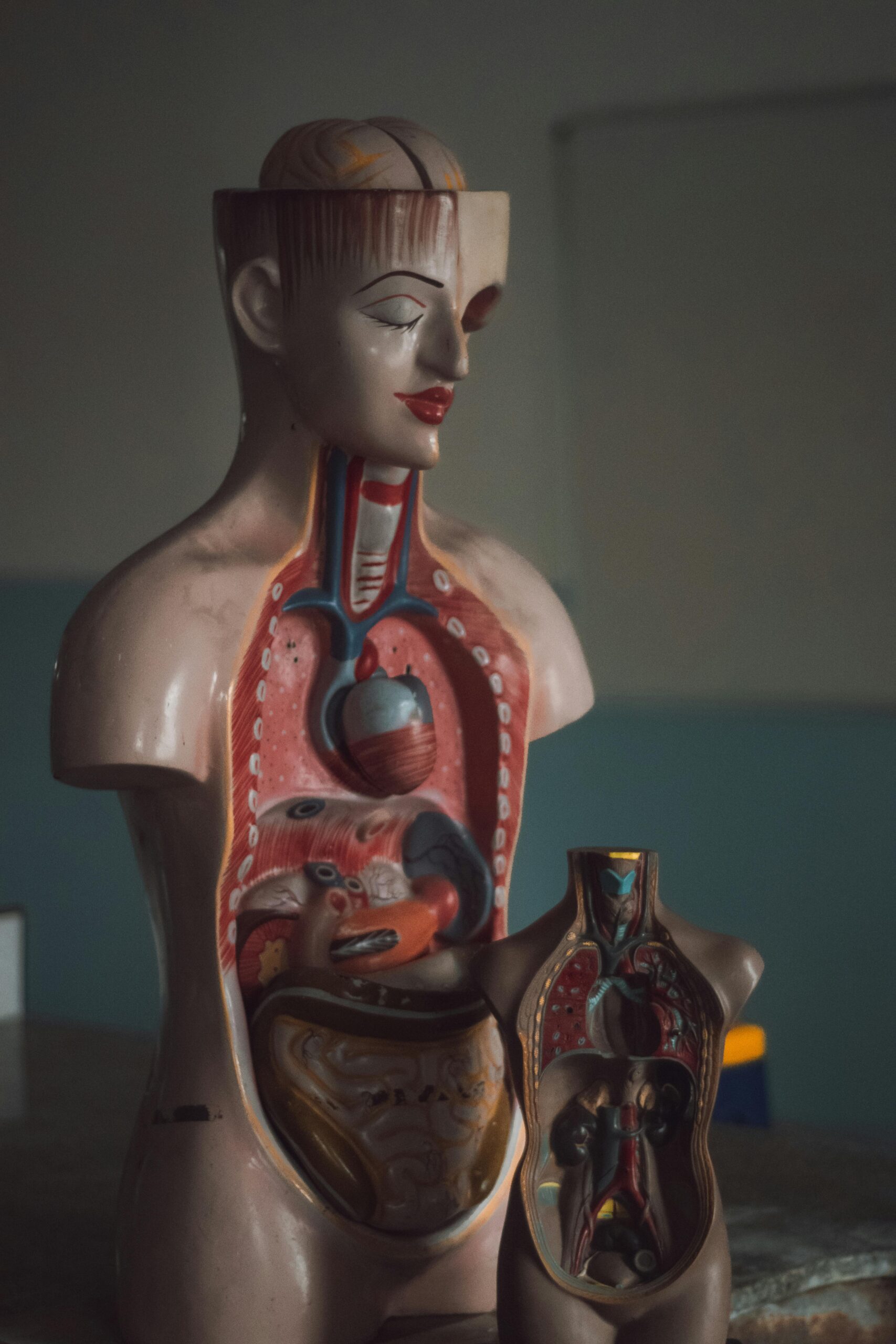
In COPD, the airflow in and out of the lungs is restricted due to inflammation and damage to lung tissues. This obstruction is typically caused by the following changes in the lungs:
- Inflammation: Chronic exposure to irritants like cigarette smoke leads to inflammation of the airways. This inflammation causes the lining of the airways to swell and produce excessive mucus, which further narrows the airways.
- Airway Remodeling: Long-term inflammation can lead to structural changes in the airways, including thickening and scarring. This makes the airways less elastic and more prone to obstruction.
- Destruction of Air Sacs: In emphysema, one of the components of COPD, the air sacs (alveoli) where gas exchange occurs are damaged. The walls between the air sacs are destroyed, reducing the surface area available for oxygen exchange and leading to difficulty breathing.
- Reduced Lung Function: As COPD progresses, the damage to the airways and air sacs results in a significant reduction in lung function, making it harder for individuals to breathe and engage in physical activities.
Key Components: Chronic Bronchitis and Emphysema
- Chronic Bronchitis: This condition is characterized by inflammation and irritation of the bronchial tubes, which carry air to and from the lungs. The inflammation causes excessive mucus production, leading to a chronic cough and difficulty breathing. Symptoms often include a persistent cough that produces sputum (mucus) and shortness of breath.
- Emphysema: Emphysema involves the gradual destruction of the alveoli, the small air sacs in the lungs where oxygen and carbon dioxide are exchanged. This destruction reduces the surface area available for gas exchange and leads to a feeling of breathlessness. Individuals with emphysema often experience difficulty exhaling fully, resulting in a buildup of air in the lungs.
Understanding these key components and how they contribute to the overall picture of COPD is essential for recognizing the disease and managing its impact effectively.
Causes and Risk Factors
Primary Causes
- Smoking: The leading cause of COPD is smoking. Cigarette smoke contains numerous toxic substances that irritate and damage the airways and lung tissues. Long-term smoking leads to chronic inflammation and destruction of the air sacs, making it the most significant risk factor for developing COPD. The risk increases with both the number of cigarettes smoked and the duration of smoking.
- Air Pollution: Exposure to air pollutants, such as industrial emissions, vehicle exhaust, and other environmental contaminants, can contribute to the development and progression of COPD. Long-term exposure to polluted air can exacerbate existing lung damage and inflammation, particularly in areas with high levels of air pollution.
Genetic Factors
- Alpha-1 Antitrypsin Deficiency: Alpha-1 antitrypsin is a protein that helps protect the lungs from damage caused by enzymes released during inflammation. A deficiency in this protein, caused by a genetic mutation, can lead to an increased risk of lung damage and emphysema. While this condition is rare, individuals with alpha-1 antitrypsin deficiency are at higher risk for developing COPD, particularly if they also smoke or are exposed to other lung irritants.
Other Risk Factors
- Occupational Exposures: Certain occupations expose individuals to dust, fumes, and chemicals that can irritate the lungs and increase the risk of COPD. Jobs in industries such as mining, construction, and manufacturing, where workers are exposed to hazardous substances, are associated with a higher incidence of COPD. Proper protective measures and monitoring are essential in these environments to reduce the risk.
- Respiratory Infections: Frequent respiratory infections, especially during early childhood, can damage the lungs and increase the risk of developing COPD later in life. Severe or repeated respiratory infections can lead to chronic inflammation and compromise lung function, contributing to the onset of COPD.
Understanding these causes and risk factors helps in identifying individuals at higher risk of developing COPD and emphasizes the importance of preventive measures, such as avoiding smoking, reducing exposure to pollutants, and managing genetic predispositions.
Symptoms of COPD
Common Symptoms
- Chronic Cough: One of the hallmark symptoms of COPD is a persistent cough that lasts for at least three months. This cough is often accompanied by the production of mucus or sputum. It typically worsens in the morning and may become more frequent as the disease progresses.
- Shortness of Breath: Difficulty breathing, especially during physical activities, is a common symptom of COPD. Individuals may experience shortness of breath even with minimal exertion, such as walking or climbing stairs. As the disease advances, shortness of breath can become more pronounced and occur at rest.
- Wheezing: Wheezing is a high-pitched whistling sound made while breathing, particularly during exhalation. It results from the narrowing of the airways due to inflammation and mucus buildup. Wheezing can be more noticeable during physical exertion or at night.
How Symptoms Progress Over Time
- Early Stage: In the early stages of COPD, symptoms may be mild and intermittent. Individuals might experience occasional coughing and shortness of breath, particularly during physical activities. The symptoms might be mistaken for normal signs of aging or other less serious conditions.
- Moderate Stage: As COPD progresses, symptoms become more persistent and severe. The chronic cough becomes more frequent, and shortness of breath occurs more regularly, even during less strenuous activities. Wheezing may become more noticeable, and individuals may start to experience fatigue and reduced exercise tolerance.
- Advanced Stage: In advanced stages of COPD, symptoms can be debilitating. Chronic cough and shortness of breath are constant and can significantly impact daily life. Individuals may struggle with basic activities, experience frequent respiratory infections, and have difficulty getting enough oxygen. Severe COPD can lead to complications such as right-sided heart failure (cor pulmonale).
Importance of Early Detection
Early detection of COPD is crucial for several reasons:
- Improved Management: Identifying COPD in its early stages allows for timely intervention, which can slow disease progression and improve quality of life. Early treatment can help manage symptoms more effectively and prevent complications.
- Enhanced Quality of Life: Early diagnosis enables individuals to make lifestyle changes and start treatments that can alleviate symptoms and enhance their ability to carry out daily activities.
- Preventing Progression: Early detection provides an opportunity to address risk factors, such as smoking cessation, and implement preventive measures that can prevent further lung damage.
- Reducing Healthcare Costs: Managing COPD early can reduce the need for emergency interventions and hospitalizations, leading to lower overall healthcare costs.
Recognizing the symptoms of COPD and seeking medical advice promptly is essential for effective management and maintaining a better quality of life.
Diagnosis and Testing
How COPD is Diagnosed
- Medical History: The diagnosis of COPD begins with a thorough medical history. A healthcare provider will ask about symptoms, their duration and severity, smoking history, exposure to environmental pollutants, and any family history of lung disease. This helps in assessing the likelihood of COPD and understanding potential risk factors.
- Physical Exam: During a physical exam, the doctor will listen to the patient’s lungs using a stethoscope to detect abnormal sounds such as wheezing or crackles. They will also check for signs of COPD-related complications and assess overall health.
- Spirometry: Spirometry is a key diagnostic test for COPD. It measures how much air a person can exhale and how quickly. The test involves taking a deep breath and exhaling forcefully into a spirometer. Results are used to assess lung function, specifically looking at the forced expiratory volume in one second (FEV1) and the forced vital capacity (FVC). A reduced FEV1/FVC ratio is indicative of obstructive lung disease like COPD.
Common Tests Used to Diagnose COPD
- Chest X-rays: A chest X-ray provides images of the lungs and can help rule out other conditions that might cause similar symptoms, such as pneumonia or lung cancer. It may show signs of hyperinflation (enlarged lungs) and changes in the lung structure associated with COPD.
- CT Scans: A computed tomography (CT) scan of the chest offers more detailed images than X-rays. It can help identify emphysema by showing damage to the air sacs and assessing the extent of lung damage. CT scans are also useful for evaluating the presence of other conditions and complications.
- Arterial Blood Gas (ABG) Test: This test measures the levels of oxygen and carbon dioxide in the blood. It helps assess how well the lungs are functioning and whether there is a need for supplemental oxygen.
- Alpha-1 Antitrypsin Testing: If there is suspicion of an inherited form of COPD, such as in cases where the disease appears early or in individuals with a family history, an alpha-1 antitrypsin test may be conducted to check for deficiencies.
Stages of COPD and How They Are Determined
COPD is classified into stages based on the severity of airflow limitation, as measured by spirometry, and the impact on the individual’s health:
- Mild (Stage 1): Characterized by mild airflow limitation. FEV1 is ≥80% of the predicted value. Individuals may have chronic cough and sputum production but might not experience significant breathlessness.
- Moderate (Stage 2): Marked by moderate airflow limitation. FEV1 is between 50% and 79% of the predicted value. Symptoms become more noticeable, and individuals may experience more frequent breathlessness and reduced exercise tolerance.
- Severe (Stage 3): Severe airflow limitation. FEV1 is between 30% and 49% of the predicted value. Symptoms are more pronounced, and individuals experience significant breathlessness, even with minimal exertion. There may be frequent exacerbations and limitations in daily activities.
- Very Severe (Stage 4): Very severe airflow limitation. FEV1 is <30% of the predicted value, or the presence of chronic respiratory failure. Symptoms are severe, with extreme breathlessness and frequent exacerbations that significantly impact quality of life. Complications, such as right-sided heart failure, may also occur.
Accurate diagnosis and staging of COPD are essential for developing an effective treatment plan and managing the disease effectively.
Treatment and Management
Medications
- Bronchodilators: These medications help to open the airways and make breathing easier. They are classified into two main types:
- Short-acting beta-agonists (SABAs): Provide quick relief by relaxing the muscles around the airways. Examples include albuterol and levalbuterol. They are typically used as rescue inhalers for acute symptoms.
- Long-acting beta-agonists (LABAs): Provide longer-lasting relief by relaxing the muscles around the airways for up to 12 hours. Examples include salmeterol and formoterol. They are used on a regular basis to control chronic symptoms.
- Corticosteroids: These anti-inflammatory medications reduce inflammation in the airways, which helps decrease mucus production and swelling. They can be taken orally (e.g., prednisone) or inhaled (e.g., fluticasone, budesonide). Inhaled corticosteroids are often prescribed for long-term management and to reduce flare-ups.
- Combination Inhalers: These contain both a bronchodilator and a corticosteroid in one device, providing both immediate and long-term relief. Examples include Symbicort (budesonide/formoterol) and Advair (fluticasone/salmeterol).
- Phosphodiesterase-4 Inhibitors: These medications, such as roflumilast, help reduce inflammation and relax the airways. They are used for individuals with severe COPD who have frequent exacerbations despite other treatments.
- Mucolytics: These help thin and loosen mucus, making it easier to expel. Examples include acetylcysteine and carbocisteine. They can be particularly useful for individuals with chronic bronchitis.
Lifestyle Changes
- Quitting Smoking: The most crucial step in managing COPD is to stop smoking. Smoking cessation slows the progression of the disease, improves lung function, and reduces the risk of complications. Various resources are available to help individuals quit, including counseling, nicotine replacement therapies, and prescription medications.
- Exercise: Regular physical activity is important for managing COPD. Exercise helps improve cardiovascular fitness, strengthen respiratory muscles, and enhance overall stamina. Pulmonary rehabilitation programs often include supervised exercise training to help individuals with COPD increase their physical activity levels.
- Healthy Diet: Maintaining a balanced diet can support overall health and help manage symptoms. Proper nutrition helps maintain a healthy weight, which can reduce the strain on the respiratory system.
- Avoiding Irritants: Minimizing exposure to environmental pollutants, allergens, and respiratory irritants can help manage COPD symptoms. This includes avoiding secondhand smoke and using air purifiers indoors.
Pulmonary Rehabilitation Programs
- Overview: Pulmonary rehabilitation is a comprehensive program designed to improve the quality of life for individuals with COPD. It includes education, exercise training, and behavioral therapy to help manage the disease.
- Components: The program typically includes supervised exercise sessions, breathing techniques, nutritional counseling, and education on managing symptoms and medications. It also provides psychological support to help individuals cope with the emotional aspects of living with a chronic illness.
- Benefits: Pulmonary rehabilitation can improve physical fitness, reduce symptoms, increase daily functioning, and enhance overall quality of life. It can also reduce hospitalizations and healthcare costs.
Oxygen Therapy
- When It’s Needed: Oxygen therapy is prescribed for individuals with severe COPD who have low levels of oxygen in the blood. It is used to ensure adequate oxygen supply to the body’s tissues and reduce strain on the heart.
- Types:
- Supplemental Oxygen: Delivered through nasal cannulas or masks, it can be used continuously or as needed based on oxygen levels.
- Portable Oxygen Concentrators: Provide a more mobile option for those needing oxygen therapy, allowing for greater flexibility and freedom.
- Benefits: Oxygen therapy can improve exercise capacity, reduce shortness of breath, and enhance overall well-being. It is also beneficial for managing complications associated with severe COPD.
Effective management of COPD involves a combination of medications, lifestyle changes, and supportive therapies. Adhering to a comprehensive treatment plan can significantly improve symptoms, quality of life, and overall health outcomes.
Living with COPD
Tips for Managing Daily Life with COPD
- Adhere to Treatment Plans: Consistently take prescribed medications and follow the treatment plan provided by your healthcare provider. Proper medication adherence is crucial for managing symptoms and preventing exacerbations.
- Monitor Symptoms: Keep track of your symptoms, including any changes in breathlessness, cough, or sputum production. This can help you notice patterns and manage flare-ups more effectively.
- Manage Your Environment: Create a comfortable and healthy living environment. Use air purifiers to reduce dust and allergens, and avoid exposure to irritants like smoke or strong fumes. Keeping your home clean and well-ventilated can also help manage symptoms.
- Stay Active: Engage in regular, moderate exercise as advised by your healthcare provider. Exercise can improve lung function, increase stamina, and enhance overall quality of life. Activities like walking, cycling, or joining a pulmonary rehabilitation program can be beneficial.
- Use Oxygen Therapy Properly: If prescribed, use supplemental oxygen as directed to ensure adequate oxygen levels and avoid complications. Understand how to operate your oxygen equipment and carry a backup supply if needed.
- Plan for Exacerbations: Have a plan in place for managing COPD exacerbations. Know when to seek medical attention and how to adjust your treatment or lifestyle to cope with worsening symptoms.
Importance of Regular Medical Check-Ups
- Monitor Disease Progression: Regular check-ups allow healthcare providers to assess the progression of COPD and adjust treatment plans as necessary. This helps ensure that symptoms are managed effectively and that the disease does not progress unchecked.
- Prevent Complications: Routine visits help identify and address potential complications early, such as infections or heart issues, before they become more serious problems.
- Review Treatment Efficacy: Regular appointments provide an opportunity to review the effectiveness of medications and other treatments. Your doctor can make adjustments based on your current condition and response to therapy.
- Update Vaccinations: Ensure that you are up to date with recommended vaccinations, such as those for influenza and pneumonia, to prevent respiratory infections that can exacerbate COPD.
Coping Strategies for Physical and Emotional Well-Being
- Breathing Techniques: Learn and practice breathing techniques such as pursed-lip breathing and diaphragmatic breathing. These techniques can help manage breathlessness and improve oxygen intake.
- Join Support Groups: Connecting with others who have COPD can provide emotional support, practical advice, and a sense of community. Support groups can be found both in-person and online.
- Manage Stress: Practice stress-reducing activities such as mindfulness, relaxation exercises, or gentle yoga. Reducing stress can help manage symptoms and improve overall well-being.
- Seek Psychological Support: COPD can affect mental health, leading to feelings of anxiety or depression. Consider speaking with a counselor or therapist to address emotional challenges and develop coping strategies.
- Educate Yourself: Stay informed about COPD and its management. Understanding the disease and its treatments can empower you to make informed decisions about your health and navigate daily challenges more effectively.
Living with COPD requires a proactive approach to managing both physical and emotional aspects of the disease. By following these tips, engaging in regular medical care, and employing effective coping strategies, individuals with COPD can improve their quality of life and maintain better control over their condition.
Prevention and Reducing Risk
Strategies to Prevent COPD
- Smoking Cessation: The most effective strategy for preventing COPD is to avoid smoking and to quit if you currently smoke. Smoking is the leading cause of COPD, and eliminating exposure to tobacco smoke significantly reduces the risk of developing the disease. For those trying to quit, various resources are available, including nicotine replacement therapies, prescription medications, and counseling.
- Avoid Exposure to Environmental Pollutants: Minimize exposure to indoor and outdoor air pollutants. This includes avoiding areas with high levels of pollution, using air purifiers indoors, and reducing exposure to industrial chemicals, dust, and fumes. If you work in an environment with hazardous substances, follow safety guidelines and use protective equipment.
- Manage Indoor Air Quality: Maintain good indoor air quality by avoiding the use of products that emit strong fumes, such as certain cleaning agents and paints. Regularly clean and ventilate your home to reduce allergens and irritants.
- Protect Yourself from Respiratory Infections: Respiratory infections can exacerbate COPD and contribute to lung damage. Practice good hygiene, such as regular handwashing, and avoid close contact with individuals who are ill. Use protective measures to avoid respiratory infections, especially during flu season.
- Adopt a Healthy Lifestyle: Maintain a balanced diet and regular exercise routine to support overall health and lung function. Proper nutrition and physical activity can help strengthen the respiratory system and improve overall well-being.
Vaccinations and Their Role
- Flu Vaccine: Annual influenza vaccination is recommended for individuals with COPD and those at risk of developing the disease. Influenza can cause severe respiratory complications and exacerbate COPD symptoms. Getting the flu vaccine helps prevent influenza-related illnesses and reduces the risk of complications.
- Pneumonia Vaccine: The pneumonia vaccine (Pneumococcal vaccine) is crucial for individuals with COPD. Pneumonia can be particularly severe for those with compromised lung function. The vaccine helps protect against pneumococcal infections, which can lead to pneumonia and other serious respiratory infections.
- COVID-19 Vaccine: For individuals with COPD, getting vaccinated against COVID-19 is also important. COVID-19 can lead to severe respiratory complications, and vaccination helps reduce the risk of severe illness and hospitalization.
- Other Vaccinations: Depending on individual health conditions and recommendations from healthcare providers, other vaccinations may also be advised. For example, the pertussis (whooping cough) vaccine may be recommended to prevent infections that can impact respiratory health.
By implementing these preventive strategies and staying up-to-date with vaccinations, individuals can significantly reduce their risk of developing COPD and related complications. Early intervention and proactive measures play a key role in maintaining respiratory health and overall well-being.
Support and Resources
Available Resources for COPD Patients and Their Families
- Support Groups: Support groups provide a valuable opportunity for individuals with COPD and their families to connect with others who understand their experiences. These groups offer emotional support, practical advice, and shared coping strategies. They can be found in local communities through hospitals, clinics, and community centers, or online through various platforms.
- Online Communities: Online forums and social media groups offer a platform for people with COPD to share their experiences, ask questions, and receive support from a broader community. Websites like Reddit, Facebook, and specialized forums like COPD.net provide spaces for individuals to connect with others who face similar challenges.
- Patient Advocacy Organizations: Many organizations offer resources, educational materials, and support services for COPD patients and their families. These organizations often provide information on disease management, treatment options, and lifestyle changes. They may also advocate for research and improved healthcare policies.
- Educational Workshops and Webinars: Many hospitals, clinics, and organizations offer workshops and webinars focused on COPD management, including topics like medication use, breathing techniques, and coping strategies. These educational events can provide valuable information and skills for managing the disease effectively.
- Counseling and Psychological Support: Professional counseling and therapy can help individuals and families cope with the emotional impact of living with COPD. Mental health professionals can assist with managing stress, anxiety, and depression related to chronic illness.
Useful Organizations and Websites for Further Information
- American Lung Association (ALA): The ALA provides comprehensive resources on COPD, including information on symptoms, treatment options, and managing the disease. Their website also offers tools for finding local support groups and educational materials. Website
- COPD Foundation: This organization focuses on supporting individuals with COPD through education, research, and advocacy. They offer resources for disease management, including online support communities and educational materials. Website
- National Heart, Lung, and Blood Institute (NHLBI): Part of the National Institutes of Health (NIH), the NHLBI provides reliable information on COPD, including research updates, treatment guidelines, and educational resources for patients and healthcare providers. Website
- Centers for Disease Control and Prevention (CDC): The CDC offers information on COPD prevention, symptoms, and management. Their website includes statistics, guidelines, and educational resources to help individuals understand and manage COPD. Website
- National COPD Awareness Campaign: This initiative provides information on COPD awareness, including resources for patients and caregivers, as well as educational materials on how to manage and prevent the disease. Website
These resources and organizations offer vital support and information for managing COPD. Engaging with these tools and communities can help patients and their families navigate the challenges of living with COPD and improve their overall quality of life.
Conclusion
Recap of Key Points
In this blog, we’ve explored essential aspects of Chronic Obstructive Pulmonary Disease (COPD), including its definition, symptoms, and the impact it has on lung function. We discussed the primary causes and risk factors, such as smoking and exposure to pollutants, and highlighted the importance of early diagnosis through methods like spirometry and imaging tests. Treatment and management strategies were covered, including medications, lifestyle changes, and pulmonary rehabilitation. We also reviewed preventive measures and resources available for support.
Encouragement to Seek Medical Advice if Experiencing Symptoms
If you or someone you know is experiencing symptoms such as a persistent cough, shortness of breath, or wheezing, it is crucial to seek medical advice. Early detection and intervention are key to managing COPD effectively and improving quality of life. Don’t hesitate to consult a healthcare provider for evaluation, diagnosis, and personalized treatment plans. Addressing symptoms promptly can help prevent the disease from progressing and reduce the risk of complications.
Call to Action for Spreading Awareness About COPD
Raising awareness about COPD is vital for improving public understanding and supporting those affected by the disease. Share information about COPD with friends, family, and your community. Encourage individuals to seek medical advice if they exhibit symptoms and support initiatives that aim to reduce the prevalence of COPD through smoking cessation and environmental protection. By spreading awareness and supporting COPD research and education, we can collectively work towards better management and prevention of this chronic condition.