Table of Contents
Autoimmune diseases are a group of disorders where the immune system mistakenly attacks the body’s own tissues. Instead of protecting the body from harmful pathogens, the immune system targets healthy cells, leading to inflammation and damage in various organs and systems. These diseases can affect almost any part of the body, including the skin, joints, muscles, and internal organs.
Autoimmune diseases are often chronic and can vary widely in severity. Common examples include rheumatoid arthritis, lupus, multiple sclerosis, and type 1 diabetes. Each condition has its unique set of symptoms and challenges, but they all share the underlying issue of an overactive or misdirected immune response.
Understanding autoimmune diseases is crucial for several reasons:
- Early Diagnosis and Treatment: Early recognition of symptoms and accurate diagnosis can lead to more effective management and improved quality of life. Many autoimmune conditions can be challenging to diagnose due to their diverse symptoms and the overlap with other diseases.
- Informed Decision-Making: Knowledge about these diseases helps patients make informed decisions about their treatment options, which can include medications, lifestyle changes, and other therapies.
- Support and Advocacy: Awareness fosters empathy and support, not only for those affected by autoimmune diseases but also for their families and caregivers. It encourages the development of better support systems and advocacy for research and improved treatments.
- Empowerment: Understanding the nature of autoimmune diseases empowers individuals to take an active role in their health management, engage in meaningful discussions with healthcare providers, and seek out necessary resources and support.
In summary, grasping the complexities of autoimmune diseases is key to managing these often debilitating conditions effectively and enhancing the overall well-being of those affected.
What Are Autoimmune Diseases?
Definition and Explanation
Autoimmune diseases occur when the immune system, which is designed to protect the body from harmful invaders like bacteria and viruses, mistakenly attacks healthy tissues. This dysfunction arises from a failure in the immune system’s ability to distinguish between foreign pathogens and the body’s own cells. Instead of targeting external threats, the immune system identifies normal, healthy cells as harmful and launches an inflammatory response against them.
This immune response can lead to chronic inflammation and damage in various organs and systems, which can impair their normal function. The exact cause of this immune system malfunction is often unclear, but it is believed to result from a combination of genetic predisposition and environmental triggers.
How Autoimmune Diseases Affect the Body
The effects of autoimmune diseases vary widely depending on which parts of the body are targeted. Common consequences include:
- Chronic Inflammation: Persistent inflammation can lead to damage and scarring of tissues and organs. For instance, in rheumatoid arthritis, inflammation primarily affects the joints, causing pain and swelling.
- Organ Damage: In some autoimmune diseases, specific organs are targeted, leading to impaired function. For example, in type 1 diabetes, the immune system attacks insulin-producing cells in the pancreas, affecting blood sugar regulation.
- Systemic Effects: Some autoimmune diseases can have widespread effects, involving multiple systems in the body. Systemic lupus erythematosus (SLE) can affect the skin, joints, kidneys, and other organs, leading to a range of symptoms.
- Functional Impairment: The ongoing damage and inflammation can lead to functional impairments, such as reduced mobility in joints or decreased organ performance, impacting overall quality of life.
Common Examples
- Rheumatoid Arthritis (RA):
- Description: RA is a chronic autoimmune disorder that primarily affects the joints. It causes inflammation, pain, and swelling in the affected areas, often leading to joint deformities and loss of function.
- Symptoms: Morning stiffness, joint pain, swelling, and fatigue.
- Lupus (Systemic Lupus Erythematosus, SLE):
- Description: Lupus is a systemic autoimmune disease where the immune system attacks multiple organs and systems, including the skin, joints, kidneys, and heart. It can be characterized by flare-ups and periods of remission.
- Symptoms: Butterfly-shaped rash on the face, joint pain, fever, fatigue, and kidney problems.
- Multiple Sclerosis (MS):
- Description: MS is a chronic autoimmune condition that affects the central nervous system (CNS), including the brain and spinal cord. The immune system attacks the myelin sheath, which protects nerve fibers, leading to disrupted nerve signals.
- Symptoms: Numbness or tingling, muscle weakness, vision problems, and difficulties with coordination and balance.
Understanding these common autoimmune diseases helps in recognizing their symptoms and the need for early diagnosis and appropriate management.
Causes and Risk Factors
Genetic Predisposition
Genetic predisposition plays a significant role in the development of autoimmune diseases. Individuals with a family history of autoimmune conditions are at a higher risk of developing similar diseases. Certain genes are associated with a higher susceptibility to autoimmune disorders by affecting immune system function and regulation. For example, specific variations in the HLA (human leukocyte antigen) genes have been linked to several autoimmune diseases, including rheumatoid arthritis and type 1 diabetes. While genetics alone do not cause autoimmune diseases, they contribute to an individual’s overall risk.
Environmental Triggers
Environmental factors can play a crucial role in triggering autoimmune responses, particularly in individuals who are genetically predisposed. These triggers include:
- Infections: Certain viral or bacterial infections may initiate autoimmune reactions. For example, the Epstein-Barr virus has been linked to an increased risk of developing multiple sclerosis and systemic lupus erythematosus. Infections may trigger autoimmune diseases by causing the immune system to mistakenly target body tissues.
- Toxins: Exposure to environmental toxins, such as heavy metals or chemicals, can contribute to autoimmune disease development. For instance, exposure to silica dust has been associated with an increased risk of rheumatoid arthritis.
Hormonal Influences
Hormones can influence the development and progression of autoimmune diseases, which may explain why some autoimmune conditions are more prevalent in women. Hormonal changes, particularly those related to estrogen, may affect immune system activity. For instance, diseases like lupus and multiple sclerosis are more common in women, and symptoms often flare during periods of hormonal changes, such as pregnancy or menopause.
Lifestyle Factors
Lifestyle factors can impact the risk and management of autoimmune diseases. Key lifestyle factors include:
- Diet and Nutrition: Certain dietary patterns or nutrient deficiencies may influence autoimmune disease risk. For example, gluten has been implicated in autoimmune conditions like celiac disease, and a diet rich in anti-inflammatory foods may help manage symptoms.
- Stress: Chronic stress can affect immune function and may contribute to the onset or exacerbation of autoimmune diseases. Stress management techniques, such as mindfulness and relaxation practices, can be beneficial in managing autoimmune conditions.
- Physical Activity: Regular physical activity is associated with better overall health and can help manage autoimmune disease symptoms. Exercise can reduce inflammation and improve joint function in conditions like rheumatoid arthritis.
- Smoking and Alcohol: Smoking has been identified as a risk factor for several autoimmune diseases, including rheumatoid arthritis and lupus. Excessive alcohol consumption may also impact immune system function and exacerbate autoimmune conditions.
Understanding these causes and risk factors can help in identifying individuals at risk, implementing preventative measures, and managing autoimmune diseases effectively.
Diagnosis of Autoimmune Diseases
Common Symptoms and Early Signs
Diagnosing autoimmune diseases can be challenging due to the wide range of symptoms and their overlap with other conditions. Common early signs and symptoms often include:
- Fatigue: Persistent and unexplained tiredness that doesn’t improve with rest.
- Joint Pain and Swelling: Especially in conditions like rheumatoid arthritis, where multiple joints may be affected.
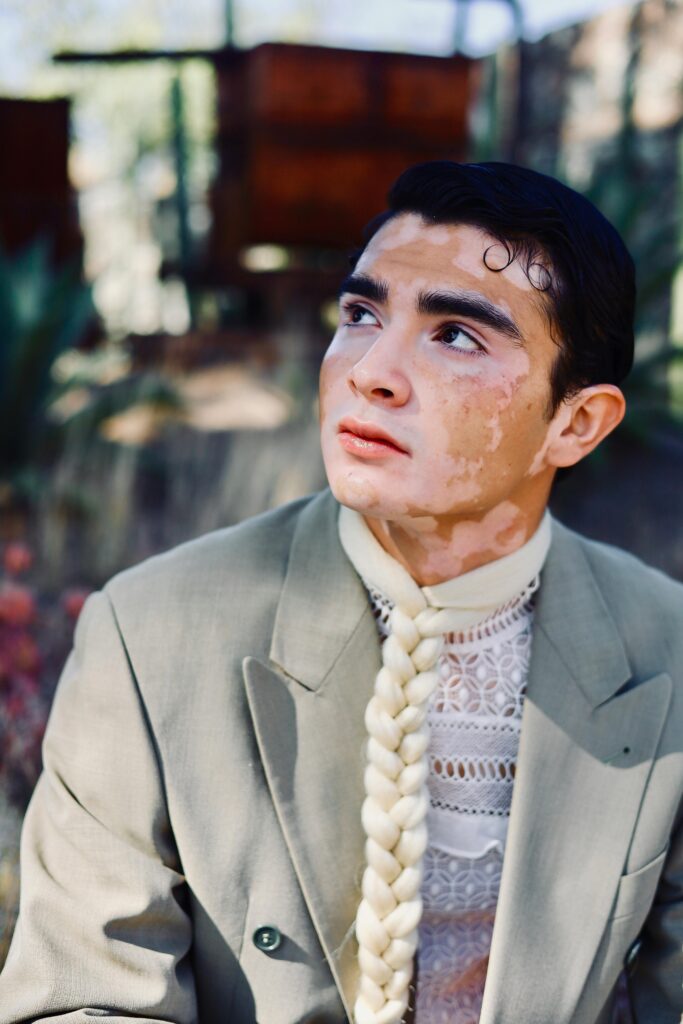
- Skin Rashes: For instance, a butterfly-shaped rash on the face is characteristic of lupus.
- Muscle Weakness: Notable in conditions like polymyositis and dermatomyositis.
- Fever and General Malaise: Common in various autoimmune diseases, indicating systemic inflammation.
- Organ-Specific Symptoms: For example, frequent urination and excessive thirst in type 1 diabetes, or visual disturbances in multiple sclerosis.
Diagnostic Process
- Medical History and Physical Examination
- Medical History: A thorough history includes evaluating symptoms, their onset, duration, and progression, as well as any family history of autoimmune diseases. The patient’s lifestyle, recent infections, and exposure to potential triggers are also considered.
- Physical Examination: The physical exam focuses on identifying signs of inflammation, joint abnormalities, rashes, or other symptoms that might indicate an autoimmune condition. This can provide initial clues and help direct further diagnostic testing.
- Laboratory Tests
- Blood Tests: These are crucial in diagnosing autoimmune diseases and often include:
- Complete Blood Count (CBC): To check for anemia or signs of inflammation.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): To assess inflammation levels.
- Autoantibody Panels: Specific tests such as antinuclear antibodies (ANA), rheumatoid factor (RF), and anti-cyclic citrullinated peptide (anti-CCP) antibodies can help identify autoimmune conditions.
- Specific Markers: For example, anti-dsDNA antibodies are associated with lupus, while anti-Smith antibodies are more specific for this condition.
- Imaging Studies
- X-Rays: Used to detect joint damage and deformities, especially in rheumatoid arthritis.
- Magnetic Resonance Imaging (MRI): Provides detailed images of soft tissues and can be used to evaluate inflammation or damage in conditions like multiple sclerosis or rheumatoid arthritis.
- Ultrasound: Can assess joint inflammation and damage, particularly useful in conditions like rheumatoid arthritis.
- Biopsy Procedures
- Skin Biopsy: In cases of suspected autoimmune skin disorders (e.g., lupus), a biopsy can help identify characteristic changes in skin tissue.
- Muscle Biopsy: Used in conditions like polymyositis to examine muscle tissue for inflammation and damage.
- Kidney Biopsy: In cases of suspected lupus nephritis, a biopsy of kidney tissue may be necessary to assess damage and guide treatment.
Challenges in Diagnosis
Diagnosing autoimmune diseases poses several challenges:
- Symptom Overlap: Many autoimmune diseases present with similar symptoms, making it difficult to distinguish between them without specific tests.
- Variable Presentation: Symptoms can vary widely among individuals and may change over time, complicating the diagnosis.
- Early Diagnosis: Some autoimmune diseases have a gradual onset, and symptoms may not be recognized until significant damage has occurred.
- Lack of Specific Tests: Not all autoimmune diseases have specific, widely available diagnostic tests, which can delay accurate diagnosis.
- Misdiagnosis: Due to symptom overlap with other conditions, autoimmune diseases may be misdiagnosed, leading to inappropriate treatments.
Effective diagnosis often requires a combination of clinical evaluation, laboratory testing, and imaging, with ongoing assessment and monitoring to refine the diagnosis and adapt treatment plans as necessary.
Treatment Options
Medications
- Anti-Inflammatory Drugs
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications, such as ibuprofen and naproxen, are commonly used to reduce inflammation, pain, and fever. They are often prescribed for conditions like rheumatoid arthritis and lupus to manage joint pain and swelling.
- Corticosteroids: Drugs like prednisone are potent anti-inflammatory agents used to quickly reduce inflammation and control symptoms during flare-ups. They are effective for conditions like lupus and vasculitis but are typically used for short-term management due to potential side effects with long-term use.
- Immunosuppressants
- Methotrexate: Often used in rheumatoid arthritis and psoriasis, methotrexate reduces immune system activity to help control inflammation and prevent joint damage.
- Azathioprine: Used to suppress the immune system in conditions like lupus and rheumatoid arthritis, it helps prevent the immune system from attacking healthy tissues.
- Cyclosporine: A potent immunosuppressant used in severe cases of autoimmune diseases to prevent organ rejection and manage diseases like psoriasis.
- Disease-Modifying Antirheumatic Drugs (DMARDs)
- Traditional DMARDs: Medications such as methotrexate, sulfasalazine, and hydroxychloroquine (used in lupus) help to slow disease progression and prevent joint damage. They are often used in rheumatoid arthritis and other chronic autoimmune conditions.
- Targeted DMARDs: Newer DMARDs, such as Janus kinase (JAK) inhibitors (e.g., tofacitinib), are designed to specifically target pathways involved in the inflammatory process, offering more precise management of autoimmune diseases.
- Biologic Agents
- Tumor Necrosis Factor (TNF) Inhibitors: Medications like adalimumab and etanercept block TNF-alpha, a protein involved in inflammation. They are used for conditions like rheumatoid arthritis and Crohn’s disease.
- Interleukin Inhibitors: These drugs target specific interleukins (e.g., IL-6 or IL-12/23) involved in the immune response, such as tocilizumab for rheumatoid arthritis.
- B-Cell Depletion Therapies: Rituximab targets and depletes B-cells, which are involved in autoimmune processes, and is used for diseases like rheumatoid arthritis and certain types of vasculitis.
Non-Pharmacological Treatments
- Physical Therapy
- Purpose: To improve mobility, strengthen muscles, and enhance joint function. Physical therapy can help manage symptoms, prevent joint deformities, and improve overall physical function in conditions like rheumatoid arthritis and multiple sclerosis.
- Techniques: Includes exercises, manual therapy, and modalities such as heat and cold therapy.
- Occupational Therapy
- Purpose: To assist individuals in performing daily activities and improving their quality of life. Occupational therapy focuses on developing or adapting skills needed for daily living and work, often through adaptive techniques or tools.
- Techniques: Includes training on joint protection, energy conservation strategies, and the use of assistive devices.
- Diet and Nutrition
- Purpose: To manage symptoms and improve overall health. A balanced diet can help reduce inflammation and support the immune system.
- Approaches: Specific dietary adjustments may include anti-inflammatory diets, avoiding known food triggers (e.g., gluten in celiac disease), and ensuring adequate intake of essential nutrients like omega-3 fatty acids and antioxidants.
- Lifestyle Modifications
- Stress Management: Techniques such as mindfulness, relaxation exercises, and cognitive-behavioral therapy (CBT) can help manage stress, which can exacerbate autoimmune symptoms.
- Exercise: Regular, low-impact exercise can help maintain joint function, improve mood, and reduce fatigue. Activities like swimming, walking, and cycling are often recommended.
Emerging Treatments and Research
- New Drug Developments: Research is ongoing to discover and develop new medications that target specific immune pathways or offer more personalized treatment options. These include new biologics, small molecule inhibitors, and advanced targeted therapies.
- Gene Therapy: Exploring how gene editing technologies, such as CRISPR, might correct genetic mutations associated with autoimmune diseases.
- Regenerative Medicine: Investigating the potential of stem cell therapies to repair damaged tissues and modulate immune responses.
- Precision Medicine: Advancing the understanding of how genetic, environmental, and lifestyle factors interact to influence autoimmune diseases, leading to more tailored and effective treatments.
- Immunomodulation: Researching methods to specifically modulate the immune system to reduce its activity in autoimmune conditions without broadly suppressing it, potentially reducing side effects.
The treatment of autoimmune diseases is highly individualized and often requires a combination of medications, therapies, and lifestyle adjustments to manage symptoms and improve quality of life. Ongoing research continues to offer hope for more effective and targeted treatments.
Living with Autoimmune Diseases
Coping with Chronic Pain and Fatigue
Living with autoimmune diseases often involves managing chronic pain and fatigue, which can significantly impact daily life:
- Pain Management: Chronic pain is common in autoimmune conditions and can be addressed through a combination of medications, physical therapy, and alternative treatments like acupuncture. Heat or cold packs, massage therapy, and relaxation techniques can also provide relief.
- Fatigue Management: Fatigue can be debilitating and may require strategies to manage effectively. This includes prioritizing tasks, balancing activity with rest, and possibly adjusting work and social activities to accommodate energy levels. Techniques like pacing, taking frequent breaks, and engaging in gentle exercise can help maintain energy levels.
Managing Symptoms Day-to-Day
Effective daily management of autoimmune disease symptoms involves a multifaceted approach:
- Medication Adherence: Taking prescribed medications consistently as directed by a healthcare provider is crucial for controlling disease activity and preventing flare-ups.
- Routine Monitoring: Regular check-ups with healthcare providers, including blood tests and other monitoring as needed, help track disease progression and adjust treatment plans accordingly.
- Self-Care Practices: Implementing self-care routines, such as practicing good sleep hygiene, engaging in stress-reducing activities, and maintaining a balanced diet, can contribute to overall well-being and symptom management.
- Adaptations and Assistive Devices: Using adaptive tools and making modifications to daily routines can help manage symptoms. For example, using ergonomic tools, mobility aids, or assistive devices can ease daily tasks and reduce strain.
Psychological Impact and Mental Health Considerations
The psychological impact of living with an autoimmune disease can be profound:
- Mental Health Challenges: Individuals may experience feelings of anxiety, depression, or frustration due to chronic pain, disability, or the unpredictable nature of autoimmune conditions. The ongoing struggle with symptoms and the need for constant management can contribute to emotional distress.
- Counseling and Therapy: Seeking support from mental health professionals, such as psychologists or counselors, can provide strategies for coping with emotional challenges. Cognitive-behavioral therapy (CBT) and other therapeutic approaches can help address negative thought patterns and improve emotional resilience.
- Support Groups: Connecting with others who have similar experiences through support groups can provide a sense of community and shared understanding. These groups offer opportunities to exchange coping strategies, share experiences, and provide mutual support.
Importance of a Support System
A strong support system is vital for managing autoimmune diseases effectively:
- Family and Friends: Support from family and friends can provide emotional comfort, practical assistance, and encouragement. Open communication about needs and limitations can help loved ones understand how to best support the individual.
- Healthcare Team: A team of healthcare providers, including primary care physicians, specialists, and allied health professionals (e.g., physical therapists, dietitians), plays a crucial role in managing the disease and providing comprehensive care.
- Community Resources: Access to community resources, such as local support groups, educational programs, and advocacy organizations, can offer additional support and information. These resources can help individuals stay informed about their condition and connect with others who are facing similar challenges.
In summary, living with autoimmune diseases requires a holistic approach that addresses physical, emotional, and social aspects. Effective management of symptoms, emotional support, and a strong network of care are essential for improving quality of life and overall well-being.
Support and Resources
Support Groups and Communities
Support groups and communities provide a valuable network for individuals living with autoimmune diseases:
- In-Person Support Groups: Local support groups offer face-to-face interactions where individuals can share experiences, exchange advice, and provide emotional support. These groups often meet regularly and may be facilitated by healthcare professionals or trained volunteers.
- Online Communities: Online forums and social media groups provide a platform for people to connect with others who have similar conditions, regardless of geographic location. These platforms allow for the exchange of information, support, and encouragement at any time.
- Specialized Organizations: Many autoimmune diseases have dedicated organizations that offer support groups, online communities, and resources tailored to specific conditions (e.g., the Lupus Foundation of America or the National Multiple Sclerosis Society).
Patient Advocacy Organizations
Patient advocacy organizations play a crucial role in supporting individuals with autoimmune diseases:
- Advocacy and Awareness: These organizations work to raise awareness about autoimmune diseases, promote research, and advocate for better treatment options and policies. They often engage in public education campaigns and legislative advocacy.
- Resources and Assistance: They provide resources such as informational brochures, educational materials, and assistance with navigating the healthcare system. They may also offer financial assistance programs, help with insurance issues, and provide access to clinical trials.
- Community Engagement: Advocacy organizations often host events, fundraisers, and conferences that allow individuals to connect with experts, learn about new research, and engage with others in the autoimmune community.
Educational Resources
Educational resources are essential for understanding and managing autoimmune diseases:
- Books and Articles: Books written by medical professionals and patient advocates provide in-depth information about specific autoimmune diseases, treatment options, and coping strategies. Articles in medical journals and popular health magazines can offer updates on research and management techniques.
- Websites and Online Portals: Reliable websites from reputable organizations (e.g., Mayo Clinic, NIH, or the American Autoimmune Related Diseases Association) provide comprehensive information on autoimmune diseases, including symptoms, treatments, and recent research.
- Workshops and Seminars: Educational workshops and seminars, often organized by hospitals, universities, or advocacy groups, offer opportunities to learn about disease management, new treatments, and self-care strategies from experts in the field.
How Friends and Family Can Help
The support of friends and family is invaluable for individuals living with autoimmune diseases:
- Emotional Support: Providing a listening ear, offering encouragement, and understanding the emotional and physical challenges of living with an autoimmune disease can make a significant difference. Empathy and patience are crucial.
- Practical Assistance: Helping with daily tasks such as grocery shopping, meal preparation, or transportation to medical appointments can alleviate some of the burdens associated with managing a chronic illness.
- Education and Awareness: Learning about the specific autoimmune disease affecting their loved one helps friends and family offer more informed support. It also helps them understand the limitations and needs of the individual.
- Encouragement of Self-Care: Supporting efforts to engage in self-care practices, including encouraging healthy lifestyle choices and adherence to treatment plans, can contribute to better disease management and overall well-being.
In summary, leveraging support groups, patient advocacy organizations, educational resources, and the assistance of friends and family can significantly enhance the quality of life for individuals with autoimmune diseases. These resources provide not only practical support but also emotional reassurance and community connection, which are essential for navigating the challenges of living with a chronic condition.
Conclusion
Recap of Key Points
Autoimmune diseases involve a malfunctioning immune system that mistakenly attacks the body’s own tissues, leading to chronic inflammation and damage. They can affect various parts of the body and present with diverse symptoms, making diagnosis challenging. Understanding the causes, such as genetic predisposition, environmental triggers, and lifestyle factors, is crucial for early detection and effective management.
Treatment options are multi-faceted and include medications like anti-inflammatory drugs, immunosuppressants, DMARDs, and biologic agents, alongside non-pharmacological treatments such as physical and occupational therapy, diet and nutrition adjustments, and lifestyle modifications. Emerging treatments and ongoing research offer hope for more effective and targeted therapies in the future.
Living with autoimmune diseases involves managing chronic pain and fatigue, coping with the psychological impact, and relying on a robust support system. Support groups, patient advocacy organizations, educational resources, and the support of friends and family play vital roles in improving quality of life and providing necessary assistance.
Encouragement for Those Affected
For those affected by autoimmune diseases, it’s important to remember that you are not alone. Many individuals and communities share similar experiences and understand the challenges you face. Embracing a proactive approach to managing your health, seeking support, and staying informed can help you navigate the complexities of your condition more effectively. Resilience and self-care are crucial, and progress in research continues to bring new hope for better treatments and improved quality of life.
Call to Action for Continued Education and Support
Continued education and support are essential for both individuals living with autoimmune diseases and the broader community. Here’s how you can contribute:
- Educate Yourself: Stay informed about your condition, treatment options, and advances in research. Knowledge empowers you to make informed decisions about your health and engage in meaningful discussions with your healthcare providers.
- Seek Support: Join support groups, connect with advocacy organizations, and reach out to your community. Building a network of support can provide emotional relief, practical assistance, and valuable information.
- Advocate for Awareness: Raise awareness about autoimmune diseases by sharing your experiences, participating in advocacy events, and supporting research initiatives. Greater awareness can lead to better resources, treatments, and support systems for everyone affected.
- Support Research: Contribute to ongoing research efforts by participating in clinical trials if possible, and support organizations that fund research and advocacy. Every contribution helps advance our understanding and treatment of autoimmune diseases.
In conclusion, managing autoimmune diseases involves a comprehensive approach that includes medical treatment, lifestyle adjustments, and emotional support. By staying informed, seeking support, and advocating for continued research, you can play an active role in improving your own health and contributing to the broader fight against autoimmune diseases.
Additional Resources and References
Links to Credible Websites
For reliable information and support regarding autoimmune diseases, consider the following websites:
- Mayo Clinic: Autoimmune Diseases Overview
Provides comprehensive information on various autoimmune diseases, including symptoms, causes, and treatment options. - National Institute of Allergy and Infectious Diseases (NIAID): Autoimmune Diseases
Offers detailed explanations about autoimmune diseases, ongoing research, and clinical trials. - American Autoimmune Related Diseases Association (AARDA): AARDA
A nonprofit organization dedicated to raising awareness and supporting research for autoimmune diseases. Provides educational materials and information on advocacy. - Lupus Foundation of America: Lupus Foundation
Provides resources, support, and information specifically for individuals affected by lupus. - National Multiple Sclerosis Society: National MS Society
Offers resources, support, and information for people living with multiple sclerosis.
Recommended Books and Articles
Books and articles can offer in-depth insights and personal experiences related to autoimmune diseases:
- “The Autoimmune Solution: Prevent and Reverse the Full Spectrum of Inflammatory Symptoms and Diseases” by Dr. Amy Myers
This book explores a holistic approach to managing autoimmune diseases through diet, lifestyle changes, and understanding autoimmune mechanisms. - “The Lupus Book: A Guide for Patients and Their Families” by Dr. Daniel J. Wallace
A comprehensive guide to lupus, offering detailed information on diagnosis, treatment, and living with the condition. - “Multiple Sclerosis: The History of a Disease” by Roy L. Swank
This book provides a historical perspective on multiple sclerosis and explores its development and treatment over time. - “Rheumatoid Arthritis: A Guide to Understanding and Managing Your Condition” by Dr. David A. Williams
A resource for understanding rheumatoid arthritis, its management, and treatment options. - “Autoimmune Disease and the Gut: A Comprehensive Guide to Diagnosis and Treatment” by Dr. Alessio Fasano
Focuses on the relationship between gut health and autoimmune diseases, offering insights into diagnosis and treatment strategies.
Contact Information for Support Organizations
For additional support and information, you can reach out to the following organizations:
- American Autoimmune Related Diseases Association (AARDA)
- Website: AARDA
- Phone: (888) 856-1237
- Email: info@aarda.org
- Lupus Foundation of America
- Website: Lupus Foundation
- Phone: (202) 349-1155
- Email: info@lupus.org
- National Multiple Sclerosis Society
- Website: National MS Society
- Phone: (800) 344-4867
- Email: contactus@nmss.org
- Arthritis Foundation
- Website: Arthritis Foundation
- Phone: (404) 965-7500
- Email: info@arthritis.org
- National Institute of Allergy and Infectious Diseases (NIAID)
- Website: NIAID
- Phone: (301) 496-5717
- Email: niaidinfo@niaid.nih.gov
These resources can provide valuable information, support, and assistance for individuals living with autoimmune diseases and their families.

